How Business Rules and Decision Tables Support Evaluation of Patient Eligibility for Publicly-Funded Vaccines
This article is based on the presentation delivered at the Business Rules Forum (2012, Ft. Lauderdale, FL). It has been written in response to the invitation from the Editorial Board of the Business Rules Journal (www.BRCommunity.com).
DISCLAIMER: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Background
There are federal, state, and local government immunization programs in the United States that provide publicly-funded vaccines to eligible patients. The largest of these programs is a federally-funded Vaccines for Children (VFC) program.[1] It is implemented by the Centers for Disease Control and Prevention (CDC) and state health departments (recipients of VFC funds). Participating healthcare providers determine each patient's eligibility for a needed vaccine, administer publicly- and privately-funded vaccine doses as appropriate, and report vaccination events and eligibility status back to immunization programs.
Immunization Information Systems (IIS)[2] help immunization programs collect and aggregate patients' eligibility information from healthcare providers. Ultimately, that eligibility information supports two objectives: 1) ensure that publicly-funded vaccines are administered only to eligible patients and 2) support vaccines' accountability measures. This article discusses a case study that applies business rules and decision table techniques to document recommendations for evaluating a patient's eligibility for publicly-funded immunization programs and private coverage.
Context model — Process diagram
Figure 1 shows a simplified process diagram depicting responsibilities of the main parties involved in evaluating a patient's eligibility for publicly-funded vaccines in context of the immunization domain.
- Immunization Program, shown at the bottom, provides publicly-funded vaccines to participating Healthcare Providers.
- Healthcare Providers, shown at the top, determine a patient's vaccination needs, screen patients to assign the appropriate eligibility/coverage category, administer publicly-funded vaccine doses if appropriate, and report vaccination events and eligibilities back to the immunization programs.
- Immunization Information Systems (IIS), shown in the middle, collect and aggregate vaccination and eligibility information from healthcare providers about vaccine doses spent (i.e., doses administered, wasted, spoiled/expired, etc.). An IIS uses that information to support accountability requirements of its immunization program and reporting needs of healthcare providers.
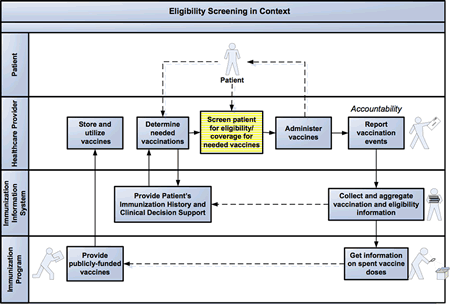
Figure 1.
Evaluating a patient's eligibility/coverage for needed vaccines in context of the immunization domain.

Domain model — Business vocabulary
Terms and definitions for this project have been captured in a domain model (Figure 2).
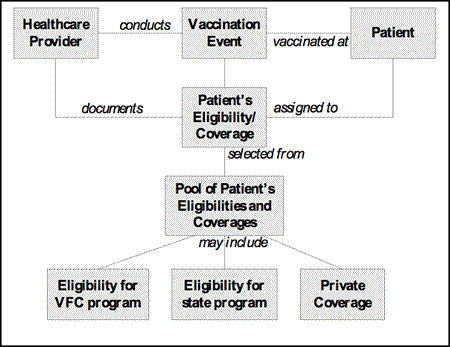
Figure 2. A fragment of the domain diagram for evaluating a patient's eligibility/coverage for needed vaccines.
Following are a few excerpts from the business vocabulary that will be used in this article:
- Eligibility — describes an association of a patient with a public immunization program, e.g., patient is eligible for the Vaccines for Children (VFC) program
- Coverage — describes an association of a patient with a private insurance or out-of-pocket pay, e.g., patient is covered by the private insurance
- Eligibility/Coverage Categories
- VFC program — Medicaid
- VFC program — American Indian and Alaska Native
- VFC program — Uninsured
- VFC program — Underinsured (i.e., patient has private health insurance, but it does not cover needed vaccines — for example, because insurance caps vaccine coverage at a certain amount)
- State program — Eligible (various degree of granularity, state-specific)
- Private coverage — Covered (private insurance or out-of-pocket pay) = VFC Ineligible
For a single vaccination event, a patient may be eligible for the VFC program, and also for a state immunization program, and also (s)he might have private insurance coverage. So, the patient's eligibility/coverage for a needed vaccine dose should be selected from a pool of available eligibilities and coverages.
Decision model — Eligibility screening conditions
Various considerations are involved when screening a patient for eligibility for public vaccines. Those considerations are very different in nature — from age, to race, to state immunization policies, and to a type of healthcare provider. Typical considerations in determining eligibility include:
- Patient's age (i.e., has patient reached 19th birthday?)
- Does patient have Medicaid (publicly-funded health insurance)?
- Is patient American Indian or Alaska Native?
- Does patient have private health insurance? If so:
- Does this private health insurance cover a needed vaccine?
- Has the private insurance vaccines-coverage cap been reached?
- Is healthcare provider of a qualified type (i.e., Federally Qualified Health Center (FQHC) or Rural Health Clinic (RHC))?
- Does state provide publicly-funded vaccines in addition to the federal VFC program?
- Does patient meet State immunization program's eligibility requirements?
On practice, these considerations can be combined in intricate combinations of multiple conditions that reflect immunization programs' policy and requirements. Decision tables and business rules were logical choices of instruments to analyze and sort out all of these aspects of the eligibility screening. Following are two guiding business rules formulated by a panel of immunization experts:
- Single eligibility/coverage should be assigned to a patient for every vaccination event/dose administered.
- Recommended hierarchy of choices for a patient's eligibility/coverage, in general, is: private insurance coverage, VFC program eligibility, State program eligibility.
Figure 3 depicts a fragment of the decision table for evaluating a patient's eligibility status. The initial version of this decision table had been developed during an in-person facilitated meeting of twelve immunization experts. It includes all conditions that were discussed above, documenting a comprehensive set of eligibility screening scenarios.
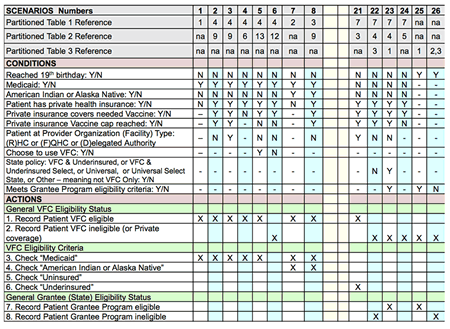
Figure 3.
A fragment of the decision table for evaluating a patient's eligibility/coverage for needed vaccines.

Abbreviations: 'Y' = Yes, 'N' = No, dash '-' means that it does not matter for the outcome of a scenario if it is 'Y' or 'N', 'X' points to actions that should be taken for this scenario, and blank indicates actions that are not applicable for this scenario.
Obviously, this decision table is big and, with added detailed conditions for state immunization programs, can quickly grow to be much larger in terms of size and complexity. And that is why we turned to the partitioning idea and approach.
Decision Model — Partitioned version
Partitioning is an established engineering approach to address complexity. A model of the complex business system gets dissected into more 'digestible' parts, allowing a practitioner to analyze each part separately and improve comprehension of the entire business.
Accordingly, the initial, large decision table has been partitioned into three smaller tables, which are associated with three logical processes on the process model (Figure 4):
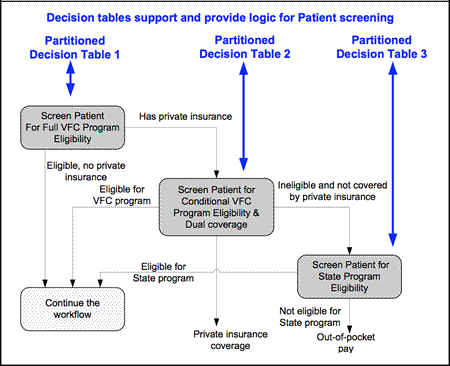
Figure 4.
Partitioned decision tables and process steps.

- Screen patient for full VFC program eligibility (decision table is presented in Figure 5). Patients who have Medicaid, are American Indians or Alaska Native, or are totally uninsured are fully eligible for all VFC program vaccines. This represents the most common, simplest case.
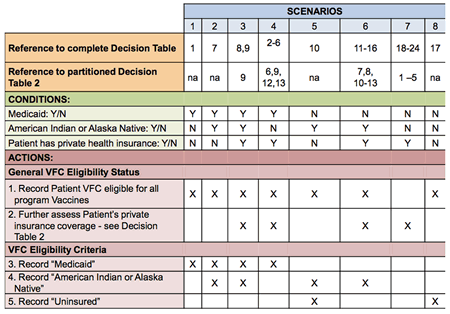
Figure 5.
Partitioned decision table 1.

- Screen patient for conditional VFC program eligibility and dual-coverage (decision table is presented in Figure 6). This process includes patients who have private insurance. Outcome depends on such factors as whether the specific vaccine needed is covered by the patient's insurance, whether the patient's insurance vaccine cap has been reached, and the type of provider (i.e., FQHC or RHC). As a result of the patient's screening for the conditional VFC eligibility, one of the three outcomes can emerge: 1) patient is VFC-eligible for a specific vaccine, 2) patient is covered by a private insurance for a specific vaccine, or 3) patient is VFC-ineligible for the needed vaccine and private insurance doesn't cover it. The first two outcomes signify the end of the patient's screening process. The third outcome leads to an additional step — patient's screening for State program eligibility.
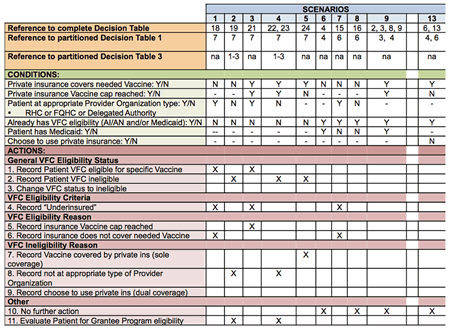
Figure 6.
Partitioned decision table 2.

- Screen patient for State program eligibility (decision table is presented in Figure 7). Each State would detail out the eligibility criteria for their specific immunization program. If the patient is determined ineligible for the State program (or if there is no State program), then he/she would have to pay out-of-pocket for the vaccine.
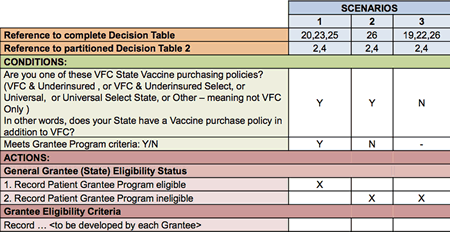
Figure 7.
Partitioned decision table 3.

This process sequence of the patient's eligibility screening (presented in Figure 4) does not create a comprehensive pool of the patient's eligibilities and coverages to select from, but rather presents a logical order of steps to determine which eligibility/coverage to use. For a given vaccine encounter, if a patient has been found to be 'fully' eligible for all VFC program vaccines, then there is no need to rescreen the patient for each vaccine needed. However, if a patient is not 'fully' eligible, then the patient needs the 'conditional' screening for each vaccine to determine if the patient's insurance covers the vaccine or not. In cases when the patient has full or conditional VFC Eligibility, no screening for the State program eligibility would be conducted. This reflects the hierarchy described above, advising that State program funds should be used only in cases when the patient is not eligible for the VFC program and does not have private insurance coverage.
Unexpected obstacle — Factor of people's perception
So, now instead of the one large table there are three smaller ones, logically connected via the associated process steps. It appeared to be a sound solution, but subject matter experts (SMEs) had difficulty using the partitioned tables, especially to trace a single operational scenario through three partitioned tables. Using the three-step process to determine eligibility turned out to be more challenging than getting it from a single pool of eligibilities and coverages. Additional illustrations and numbering schemes that link scenarios in decision tables together did not substantially help SMEs navigate these tables. We ended up going back to the original 'all-inclusive' decision table (shown in Figure 3), and placed partitioned tables (shown in Figures 5-7) in the appendix of the recommendations document.
Conclusion
Decomposition is a fine and a proven technique but it can cause problems. In this case, the partitioning of a large, 'all-inclusive' decision table into more manageable, smaller decision tables, while being conceptually sound, led to a prescriptive set of associated process steps and resulted in challenges of acceptance by SMEs and users. Such an outcome when using the decomposition approach is in line with experience of other practitioners. For example, Alec Sharp in his 2011 workshop From Process Redesign to IT Requirements, stated that "Carving up a single process into multiple, one-page diagrams (effectively, a decomposition) can destroy the story." Lesson learned: a logically sound and elegant solution is not always the most practicable one.
In spite of that decomposition-related disappointment, the overall outcome of implementing the decision tables and business rules techniques in our public health settings resulted in a positive outcome. The recommendations we developed[3] are used by many immunization information systems in the United States.[4]
Acknowledgements
Authors would like to acknowledge:
- Our colleagues from state immunization information systems, state immunization programs, Vaccines for Children (VFC) program, software vendors, and public health consultants who volunteered to participate in the experts' panel and contributed greatly to the development of recommendations and logic for evaluating a patient's eligibility.
- Team from Advanced Strategies, Inc., especially Gail DeCosta who developed initial version of decision tables during the facilitated meeting of immunization subject matter experts.
[1] Vaccines for Children Program, URL: http://www.cdc.gov/vaccines/programs/vfc/index.html ![]()
[2] Immunization Information Systems, URL: http://www.cdc.gov/vaccines/programs/iis/about.html ![]()
[3] AIRA Modeling of Immunization Registry Operations Work Group (Eds). Immunization Information System Collaboration with Vaccines For Children Program and Grantee Immunization Programs. Atlanta, GA: American Immunization Registry Association. April, 2011. URL:
http://www.immregistries.org/AIRA-MIROW_IIS-VFC_Best_Practice_Guide_04-14-2011.pdf ![]()
[4] Williams W, Lowery E, Lyalin D, Lambrecht N, Riddick S, Sutliff C, Papadouka V. "Development and Utilization of Best Practice Operational Guidelines for Immunization Information Systems." Journal of Public Health Management and Practice. 2011; 17(5): 449-456. ![]()
# # #
About our Contributor(s):
Online Interactive Training Series
In response to a great many requests, Business Rule Solutions now offers at-a-distance learning options. No travel, no backlogs, no hassles. Same great instructors, but with schedules, content and pricing designed to meet the special needs of busy professionals.